Abstract
Background: Pain crisis is the most frequent reason for admission in children with sickle cell disease (SCD). Frequent hospitalizations are associated with school absenteeism, emotional distress, and financial hardships. There is limited literature on initiatives to decrease admissions and hospital days in SCD pain crises. Prior studies have shown that individualized pain plans in emergency rooms can decrease admission rates and that a multidisciplinary approach with provider and patient education and close follow up can decrease 30-day readmission rates. Our goal was to decrease hospital days for pain crisis admissions by 40% over a 5-year period using a multidisciplinary approach.
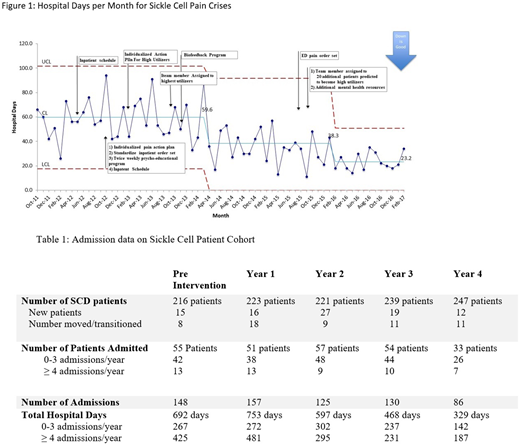
Methods: From September 2011 to August 2016 a multidisciplinary quality improvement project was conducted. A Plan-Do-Study-Act methodology was used. Five key drivers were identified and nine interventions were implemented. Interventions for the entire cohort included individualized home pain plans, emergency room and inpatient order sets, inpatient daily schedules, and a psychoeducation and biofeedback program. High utilizers, defined as ≥ 4 admissions per year, had an individualized SCD plan and were assigned a mental health provider. The high utilizer group was expanded to include at risk patients (3 admissions per year). Data was analyzed for all patients age 0-21 years admitted for SCD pain crises. The primary measure was hospital days, with 30-day readmission rate as a balancing measure.
Results: 216 SCD patients were followed in 2011, with a 14% increase over the five year study period. From this cohort, a total of 122 patients were admitted for pain crises during this time. 48% of admitted patients were male, with a mean age of 10.68±5.65 years, and 72% had hemoglobin SS disease (16% SC, 5% Sβ0, 7% Sβ+). As shown in Table 1, the number of patients admitted decreased from 55 patients (25.4% of total SCD patients) in the pre-intervention period to 33 patients (13.3% of total SCD patients) in the final year of the intervention (p = 0.0014). The number of admissions decreased from 148 admissions in the pre-intervention period to 86 admissions in the final year of the intervention (54.7% decrease). The number of hospital days decreased by 61% from 59.6 days per month in the pre-intervention period to 23.2 days per month in the final year of the intervention (p < 0.0001). Number of high utilizers decreased from 13 patients in the pre-intervention period to 7 patients in the final year of the intervention. There was a 66% reduction in the number of hospital days in the high utilizer group compared to a 47% reduction in the low utilizer group. The 30-day readmission rate decreased from 33.9% pre-intervention to 19.4% in the final year of intervention. Special cause variation was first achieved in April 2014, 18 months after the start of all interventions, with a shift of the centerline from 59.6 days/month to 38.3 days/month and again in February 2016 with a decrease to 23.2 days/month (Figure 1). There was special cause variation in 30-day readmissions in April 2014 with a centerline shift in the 30-day readmission rate from 33.9% to 19.4%. The baseline direct hospital cost for SCD admissions was $909,000 per year. In the final year of the project, the average cost was $353,880 per year, with an overall annual savings of $555,120 in direct hospital costs.
Conclusion: In this single center study, the multidisciplinary approach of effective home, emergency room, and inpatient pain management combined with increased mental health services for higher risk individuals proved to be effective in decreasing SCD pain crisis admissions and hospital days. A dedicated team effort with simple interventions had a significant impact on the well-being of the entire SCD population, but especially those who were more frequent utilizers of the healthcare system, while decreasing hospital costs, and can serve as a model for other institutions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.